
Manage FF&E specification, procurement, and product data at scale. Take on bigger projects with confidence and grow your firm with Fohlio. Schedule a demo or book a consultation with one of our account managers to explore these features today.
It might seem counterintuitive at first, but being in a hospital actually increases the chances of infection. There’s even a term for these contaminations that are specifically picked up in infirmaries, and a body of literature dedicated to their invention: healthcare-associated infections.
How bad is this phenomenon?
Well, 5-10% of hospitalized patients develop HAI, which also causes 99,000 deaths per year.
In fact, HAIs are such a big problem that the Healthcare Associated Infections Organized (HAIO) was created “to minimize and/or eradicate the spread of Healthcare Associated Infections through the use of architecture, design, and construction, including their impact on operations and maintenance.”

While there’s never a bad time to discuss the design of healthcare environments and how they aid in (or hinder) preventing the spread of infection, it’s also especially relevant now that hospitals all over the world are struggling to cope with the fast-spreading COVID-19.
In the case of highly infectious diseases like this, interrupting the chain of transmission is crucial. It’s why quarantines and COVID-specialized hospitals are at the forefront of the medical community’s response.
And while hospitals mostly rely on active protocols like hand-washing and surface cleaning to prevent the spread of infections, there are also a lot of passive strategies that can help.
We’ve gathered some best practices for designing to prevent healthcare-associated infections.
Healthcare Layout Design Strategies to Prevent Infection
In 2015, the HAIO proposed a challenge to Boston’s top healthcare design firms: “Design the ideal patient room to assist in the reduction of HAIs.”
Seven design firms submitted entries, but it was eventually decided that instead of selecting one winner, all the best ideas would be incorporated into the final design.
Ten prototype units of the design were opened at Brigham and Women’s Hospital’s Bone Marrow Transplant Unit in 2018.
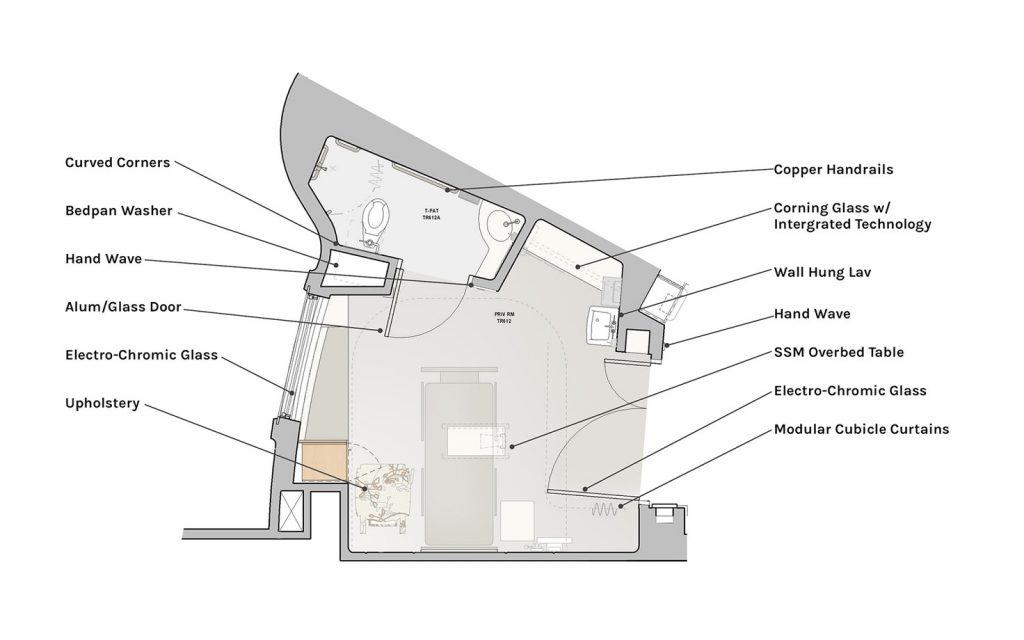
The rooms use visual cues that prompt desirable behavior (like a conspicuous sign that reminded staff to wash their hands). They also use materials that discourage the growth of pathogens, plus technology that minimizes hand contact.
Finally, the rooms utilize some specific zoning strategies. For example, the hand-washing sink is separated from work zones in order to prevent splash and cross-contamination. The area for washing bedpans is self-contained for the same reason. And finally, the patient’s bed is generously distanced from these two areas.
Utilizing Specialized Units to Avoid Contamination
Just as zoning is important to keeping patients away from pathogens, it’s also crucial to enforce separate zones to accommodate different patient conditions.
In Wuhan, for example, the two hospitals specifically built to handle COVID-19 cases have rooms with negative air pressure. This means air goes into the room but not out into the general populace, thus reducing the risk of spreading the virus.
On the other hand, most hospitals have protective environments (aka PEs) where high-risk, immunocompromised patients are cared for. These include intensive care units (ICUs) and operating rooms.
In this case, these rooms have positive room air pressure relative to its surroundings. This prevents outside air from entering, which reduces the risk of outside pathogens reaching the patients.
Incoming air is almost always filtrated as well using HEPA filters. The air flow is often directed, too: The supply comes from one side of the room to the patient and then exits through an exhaust, instead of being recirculated inside.
A relatively new type of specialized area has come about as the direct result of SARS in 2003. At the Singapore General Hospital, for example, patients are screened at points of entry and in the emergency departments. Besides being made to answer a questionnaire, body temperature is also recorded, in order to identify high-risk patients as early as possible. Anyone with a fever and a positive response to travel in high-risk areas are moved to the febrile area, even before formal triage is performed.

Besides separating potential high-risk patients from the general population, there are a few other differences between the febrile areas and other rooms. Similar to the rooms in Wuhan, these also have negative air pressure. The ventilation is also designed to dilute droplets, typically the mechanism by which SARS, COVID-19, and similar diseases are spread. Lastly, infected air from patients is not allowed to stay in the area, nor circulated through other rooms. Instead, it’s filtered to the outside environment.
Read: Healthcare Design: Spotting the Differences Between Nursing Homes and Outbreak Facilities
Selecting Materials That Help Prevent Healthcare-Associated Infections
While it’s still not clear exactly how long the novel coronavirus can live on different surfaces, there have been numerous studies on the lifespan of other pathogens. For example, MRSA can live for “11 days on a plastic patient chart, more than 12 days on a laminated countertop, and nine days on a cloth curtain.”
Of course, there’s no way to eliminate all pathogens from all hospitals all the time. Even proper hand-washing and disinfecting provide no guarantees.
Still, anything that reduces buildup and makes it easier to interrupt the transmission of infections will help.
For Wilsonart, a manufacturer of engineered surfaces, materials have to pass the “three D’s” of selection: disinfectability, durability, and design. Disinfectability refers to a material’s ability to withstand the harsh chemicals and technology necessary to kill pathogens. Durability, on the other hand, is its capacity to prevent cracks and chips — flaws that allow dirt to gather and make it harder to clean. Lastly, materials have to have an aesthetic that allows them to promote health and well-being.
For example, Construction Specialties, Inc. produces PVC-free wall and door protection products called Acrovyn. The wall sheeting and panels, corner guards, crash rails, handrails and door-frame protection are impact-resistant and embedded with color.
Sedia Systems Inc. in Chicago produces the JumpSeat Wall, which is a “low-profile, wall-mounted foldable chair,” according to their marketing manager. Its wood finish can be cleaned with a diluted bleach solution and includes antimicrobial protection.
Linda Lybert provides a list of questions to ask when selecting materials: What will it take to clean this surface? Can it be cleaned with the products the facility is currently using? Has it been tested to verify that hospital-grade disinfectants can be used without causing damage? How often will it need to be cleaned and disinfected to reduce bioburden and prevent cross-contamination?
Have you designed hospitals, senior nursing homes, emergency hospitals, or all of the above? What design strategies did you utilize to prevent the spread of infection?
Read: 3 Cost-Saving Reasons Your Hospitality Design and Procurement Teams Should Collaborate Better
Fohlio allows you to manage your entire team and all your workflows in one place. With Fohlio, you can specify, procure, and more on one platform: Collaborations are easy and workflows are much more efficient than ever before! Get your free trial today — so you can design and build more profitable projects.
Featured image from SmithGroup.
Sources:
Guidelines for Environmental Infection Control in Health-Care Facilities
Healthcare’s most pressing infection prevention challenges
Working to Reduce HAIs: How Design Can Support Infection Control and Prevention
Hospital design for better infection control
Furnishings and materials to aid infection prevention
Seven aspects of material selection
Designing for Infection Prevention
Safe design of healthcare facilities
Engineering Infection Control Through Facility Design
Expore Fohlio
Learn how to:
- Save days of work with faster specification
- Create firm-wide design standards
- Automate and centralize procurement
- Keep your whole team on the same Page
- Manage product data
- Track budget against cost in real time.
- Prepare for asset valuation
Published Mar 10, 2020

